The Healthy Heart
THE HEART AS A PUMP
The heart is a muscular pump that circulates blood around your body. It is composed of 4 chambers and 4 valves that work in concert to pump blood to the lungs to collect oxygen which is then delivered to the rest of the body.
The left and right atria are positioned side by side and form the heart’s upper chambers, while the left and right ventricles form the lower chambers.
- The “right heart”. The right atrium receives blood as it returns from the body and channels it through a valve into the right ventricle. The right ventricle then pumps blood to the lungs where it collects oxygen to deliver to the rest of the body.
- The “left heart”. The left atrium receives blood from the lungs and channels it through another valve into the left ventricle. The left ventricle then pumps blood to the rest of the body via the arteries. The left ventricle is the strongest and most important chamber of the heart and is responsible for generating the blood pressure.
THE HEART’S ELECTRICAL SYSTEM
“Your heart’s rhythm is regulated by an electrical system.”
The heart has an electrical system that coordinates its pump function.
Every normal heartbeat starts with an electrical signal generated by the heart’s own pacemaker or “spark plug”, called the sino-atrial node (SA node), or simply the sinus node.
The sinus node sets the heart’s rhythm and rate by firing 60 to 100 times a minute. It fires more rapidly during exercise and stress, and slows down during rest or sleep.
[MedMovie Image: Electrical System]
Each electrical impulse from the sinus node spreads through the right and left atria like a ripple in a pond, causing the chambers to contract. The impulse reaches the atrio-ventricular node (AV node) in the centre of the heart, and is then transmitted into the lower chambers via specialized electrical “cables” that course through the right and left ventricles.
The AV node is a critical structure in the heart as it is the only electrical connection between the upper and lower chambers. As the electrical impulse courses through the ventricles, it causes them to contract and to pump blood to the lungs and the body.
“Sinus rhythm means normal rhythm.”
The sinus node, the AV node, and the specialized electrical cables of the lower chambers of the heart need to function correctly to generate the normal heartbeat. When the normal sequence of electrical activity is disrupted, an abnormal heart rhythm will result.
We can determine if the heart is in normal rhythm by performing an ECG test. Normal rhythm is called “sinus rhythm”, in reference to the SA node (sinoatrial node) which normally controls the heart’s rhythm.
WHAT IS AN ARRHYTHMIA?
“An arrhythmia is an abnormal heart rhythm.”
Abnormal heart rhythms are called arrhythmias. There are many types of arrhythmias which may arise for different reasons. During an arrhythmia, the sinus node is no longer in normal control of the heartbeat. Abnormal electrical activity within the heart may cause the heart to beat too slowly (bradycardia), too quickly (tachycardia), or even irregularly.
Arrhythmias may cause palpitations, breathlessness, fatigue, dizziness, and fainting spells. Some arrhythmias have more serious consequence including heart failure, stroke, and cardiac arrest.
Individuals who are otherwise healthy and free of heart disease may experience arrhythmias. However, those with underlying heart disease are at the highest risk. Common heart problems such as heart attack and heart failure are important causes of arrhythmias.
WHAT ARE ECTOPIC HEARTBEATS?
An ectopic heartbeat is an “out-of-place” heartbeat due to a single muscular twitch of the heart. Ectopic heartbeats occur in all individuals, and are almost always harmless.
“Ectopic beats are almost always harmless, requiring no treatment at all.”
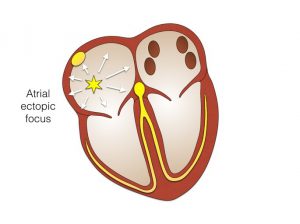
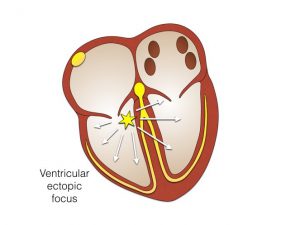
The heart normally beats to a regular rhythm. Occasionally, a heartbeat will occur ahead of time. This happens when a small cluster of muscle cells in the upper or lower chambers sends out a single electrical impulse early and out of rhythm.
The heart normally responds to this with a momentary pause before resuming its normal regular rhythm. Ectopic heartbeats generally go unnoticed. Some individuals experience the pause as a “missed beat”. Others feel a “thump”, since the following beat is larger and stronger than usual. These sensations are often more prominent when resting quietly or lying down.
The 2 most common types of ectopic heartbeats are
- Atrial ectopics arise from the heart’s upper chambers, and are also termed premature atrial contractions (PACs).
- Ventricular ectopics arise from the heart’s lower chambers, also termed premature ventricular contractions (PVCs).
WHY DO I HAVE ECTOPIC HEARTBEATS?
Ectopic heartbeats are usually nothing to worry about. They occur in perfectly health individuals for no reason at all, and they can occur at any age.
In some cases, ectopic beats may reflect
- Normal physical states such as exercise, stress, pregnancy, menopause, and ageing
- Fluctuations in potassium and magnesium levels in the blood
- Intake of caffeine, alcohol, or recreational drugs
- Effects of medications such as asthma puffers and nasal decongestants
Conditions affecting heart muscle including prior heart attack and heart failure
WHAT ARE THE CONSEQUENCE OF ECTOPIC HEARTBEATS?
Atrial ectopic beats. These rarely cause problems beyond occasional palpitations. In some cases, rapid runs of atrial ectopy can lead to an rapid irregular arrhythmia called paroxysmal atrial fibrillation.
Ventricular ectopic beats. These also rarely cause problems beyond occasional palpitations. In some individuals with frequent ventricular ectopic beats, the abnormal beats result in weakening of the heart muscle which may progress to heart failure. Occasionally there may be runs of many ectopic beats in a row and this is called ventricular tachycardia. Early evaluation and sometimes ongoing monitoring is important to identify those needing treatment for deteriorating heart function.
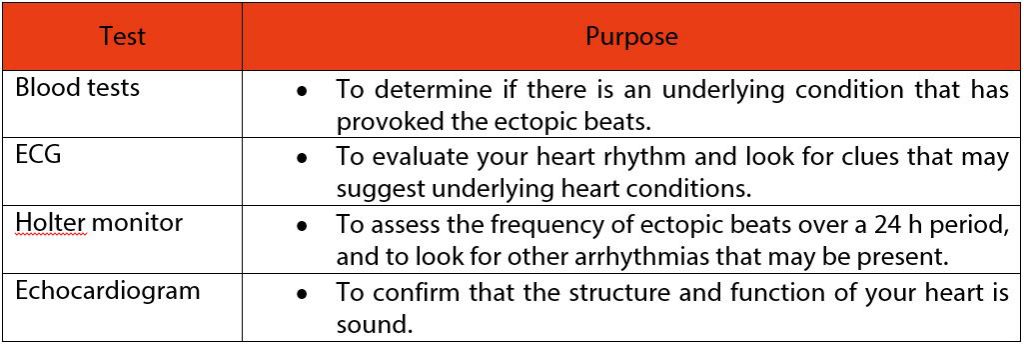
WHAT TESTS DO I NEED IF I HAVE ECTOPIC HEARTBEATS?
DO I NEED TREATMENT FOR ECTOPIC HEARTBEATS?
If there is an underlying medical condition that is causing your ectopic heartbeats, then this needs to be addressed.
Atrial ectopic beats require no specific treatment. At times there may be troublesome or intrusive symptoms. These will often wax and wane according to changes in lifestyle and will eventually run their course. If required, medications are effective at suppressing symptoms.
Ventricular ectopic beats require no specific treatment if they are infrequent and asymptomatic, and if the heart is otherwise in good condition.
For frequent or symptomatic ventricular ectopic beats, options include:
- Observation, with periodic check-ups to review your heart function with echo and holter monitoring.
- Medications such as beta blockers or calcium channel blockers to suppress ectopic beats.
Catheter ablation to eliminate the ectopic beats altogether, especially if they are associated with ventricular tachycardia.
MAINTAINING A HEALTHY HEART
Maintaining a healthy heart reduces your lifetime risk of heart disease and arrhythmias.
- Eat a healthy low-fat, high-fibre diet with plenty of vegetables, fruits, and other vitamin-rich foods.
- Commit to planned exercise for at least 30 min, 5 days per week. Cleaning the house and getting the groceries are usual physical activities that are considered incidental exercise, not planned exercise. Planned exercise means repetitive physical activity for the purpose of improving physical fitness.
- Maintain a healthy weight. Weight yourself regularly and aim for a body mass index (BMI) within the healthy range. Your BMI is your weight (kg) divided by the square of your height (m).
- Stop smoking and avoid second-hand smoke (smoke from other people). Tobacco contributes to as much as one-third of all heart disease.
- Avoid or limit the intake of caffeine, alcohol, and other substances that may contribute to arrhythmias or heart disease.
- Avoid unnecessary stress, such as anger, anxiety, or fear. Find ways to manage stressful situations that cannot be avoided.
Here are some further tips on living a “heart healthy” life:
- If you have a heart condition, follow-treatment plans, and take all your medications regularly as prescribed.
- Have regular physical exams with your GP and report any unusual symptoms you have.
- Talk to your GP about lifestyle changes and treatments that address your cardiac risk factors.
For more information, read our section on Preventing Heart Disease.